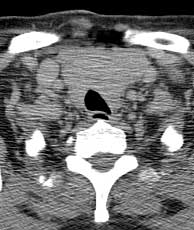
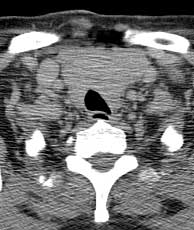
Diagnosis: Papillary thyroid carcinoma
Papillary thyroid carcinoma accounts for 3/4 of all thyroid malignancies and has the highest incidence of nodal metastasis with 1/2 patients presenting with metastases at diagnosis. On CT they may contain hemorrhage, cystic components and calcifications. Invasion of the trachea and nodal disease may also be seen. Follicular carcinoma of the thyroid gland is much less common but has a higher tendency to metastasize. On CT it is usually solid and may have calcifications. Medullary thyroid carcinoma is an uncommon tumor which may be familial and is associated with multiple endocrine neoplasia. Anaplastic thyroid carcinoma usually has necrosis and calcifications with nodal metastases. Lymphomas of the thyroid gland may occur but tend to be hypodense on CT. Necrosis and calcification are uncommon. Other entities to consider in the differential of thyroid mass include multi-nodular goiter which typically has mixed areas of solid tissue with cystic components and functioning or non-functioning thyroid adenomas. Parathyroid adenomas and carcinomas are also in the differential for thyroid region masses. Related Cases
Som PM, Brandwein M, Lidov M, et al. The varied presentations of papillary thyroid carcinoma cervical nodal disease: CT and MR findings. AJNR, Jun 1994; 15(6):p1123-8.